A lot of people have metabolic syndrome and do not know it. You might feel mostly fine, yet a few quiet changes in your blood pressure, waistline, cholesterol, or blood sugar can quietly raise your risk of heart disease, stroke, and type 2 diabetes.
In fact, about one in three adults in the United States meets the criteria for metabolic syndrome as of 2024, according to Cleveland Clinic (Cleveland Clinic). That makes it very common, but also very treatable if you catch it early.
This guide walks you through what metabolic syndrome is, why it happens, and the realistic steps you can take to prevent or reverse it.
What metabolic syndrome actually is
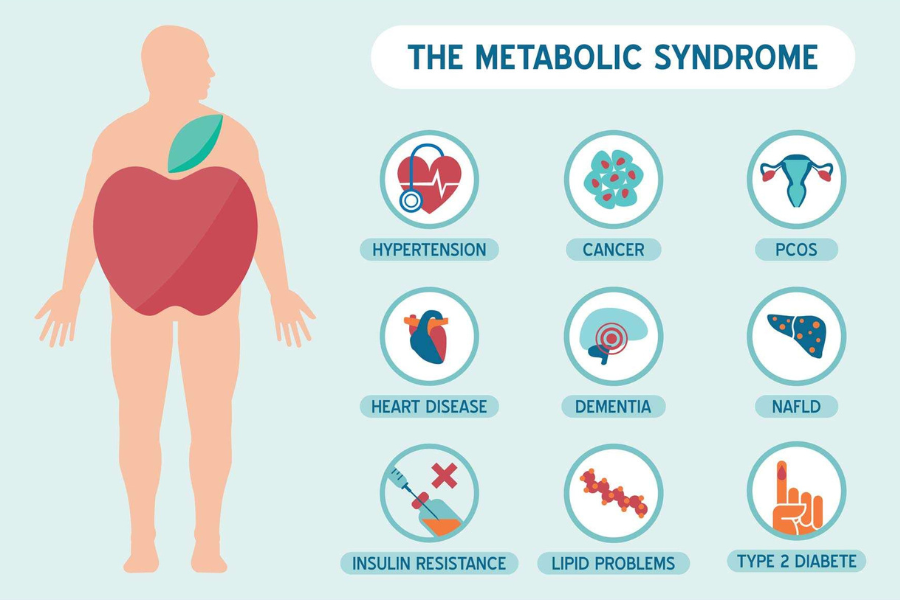
Metabolic syndrome is not one single disease. It is a cluster of conditions that tend to occur together and that, together, dramatically increase your risk of serious problems.
You are considered to have metabolic syndrome if you have at least three of the following, or you are taking medicine to control them:
- High blood pressure
- High blood sugar
- Excess fat around your waist
- High triglycerides
- Low HDL cholesterol, the so-called good cholesterol
This definition is consistent with guidance from Mayo Clinic and the National Institutes of Health (Mayo Clinic, Mayo Clinic).
You do not need to wait until you have three of these before you take action. Even one or two are a sign that your metabolism is under strain and that your long term risk is higher than it needs to be.
Why metabolic syndrome is more common than you think
You might imagine metabolic syndrome as something rare or extreme, but it is not. Mayo Clinic notes that up to one third of adults in the United States are affected, and even a single related condition raises your risk of serious disease (Mayo Clinic).
There are a few reasons it is so widespread today. Many daily routines involve long periods of sitting, easy access to ultra processed foods, chronic stress, and short sleep. Over time, these habits encourage weight gain around your midsection, higher blood pressure, and creeping blood sugar levels.
Metabolic syndrome typically shows up in people who are overweight or obese, inactive, or who have insulin resistance, where your cells do not respond properly to insulin (Mayo Clinic). Genetics and age can make you more vulnerable, but your daily choices still play a powerful role.
The root cause: insulin resistance
At the center of metabolic syndrome is insulin resistance. Insulin is a hormone that helps move sugar from your blood into your cells so you can use it for energy. When you are insulin resistant, your muscle, fat, and liver cells do not respond to insulin as well as they should.
Cleveland Clinic explains that when this happens, your blood sugar stays higher, and your pancreas responds by making even more insulin, a state called hyperinsulinemia (Cleveland Clinic). Over time, this combination strains many systems in your body.
Insulin resistance tends to:
- Raise your blood sugar, which can lead to prediabetes and type 2 diabetes
- Push your body to store more fat around your waist
- Change how your body handles fats like triglycerides and cholesterol
- Contribute to higher blood pressure
You usually cannot feel insulin resistance directly. Instead, you see its fingerprints in your lab results, your waist measurement, and your energy levels.
How metabolic syndrome affects your body
Metabolic syndrome does not cause one single symptom that you can easily recognize. Many people feel normal. The problem is what is happening quietly inside your blood vessels and organs over time.
According to Cleveland Clinic and Mayo Clinic, having metabolic syndrome means a much higher risk of (Cleveland Clinic, Mayo Clinic):
- Heart disease and heart attacks
- Stroke
- Type 2 diabetes
- Atherosclerosis, or plaque buildup in your arteries
- Organ damage, such as to your kidneys
Carrying more weight around your waist seems to be particularly important. People with metabolic syndrome usually have an apple shaped body, with more weight around the middle, which is linked to higher risk of diabetes and heart disease. A pear shaped body, with more weight around the hips, does not carry the same level of risk (Mayo Clinic).
The reassuring part is that this risk is not fixed. Early intervention can reverse metabolic syndrome and lower your chance of these complications (Cleveland Clinic).
Warning signs to watch for
Because metabolic syndrome is mostly silent, regular checkups matter. You cannot rely on how you feel. Instead, you can ask your health care provider about these measures:
- Waist circumference
- Blood pressure
- Fasting blood sugar or A1C
- Fasting triglycerides
- HDL cholesterol
If three or more are outside the healthy range, or you are on medicine for them, the National Institutes of Health definition says you meet the criteria for metabolic syndrome (Mayo Clinic).
You might also notice subtle clues, such as needing larger belt sizes over time, feeling more tired after meals, or being told repeatedly that your numbers are a bit high but not quite in the disease range. These are early nudges that your metabolism could use some support.
Why early treatment makes such a difference
The main goal of treating metabolic syndrome is to lower your risk of heart disease and to prevent type 2 diabetes if you do not have it yet. If you already have diabetes, the goal is to control all your risk factors to protect your heart and blood vessels (NHLBI).
The good news is that small improvements can have a big payoff. The National Heart, Lung, and Blood Institute highlights that losing just 3 to 5 percent of your body weight can help improve cholesterol and diabetes related risk factors that increase heart disease risk (NHLBI). Mayo Clinic notes that the same modest weight loss can reduce insulin resistance, lower your chance of diabetes, and bring down blood pressure (Mayo Clinic).
You do not have to reach a perfect number on the scale to see benefits. Even a relatively small change, if you keep it off, can shift your trajectory.
Lifestyle changes that make the biggest impact
Heart healthy lifestyle changes are the first line of treatment for metabolic syndrome. They are often enough to control or even reverse it, especially when you start early (NHLBI).
Move your body most days
Aim for at least 30 minutes of physical activity on most days of the week. Health experts say this can be as simple as brisk walking, and you can break it into shorter chunks throughout the day if you prefer (Mayo Clinic).
You might:
- Walk during lunch instead of scrolling on your phone
- Take the stairs instead of the elevator when you can
- Park a little farther and turn errands into short walks
Over time, regular movement improves insulin sensitivity, lowers blood pressure, supports weight loss, and boosts mood.
Shift your eating pattern, not just single foods
You do not need a complicated diet to support metabolic health. Two eating patterns in particular have strong evidence:
- The DASH diet
- The Mediterranean diet
Both emphasize more whole, minimally processed foods and fewer refined products. They usually include plenty of vegetables, fruits, whole grains, beans, nuts, healthy fats, and modest amounts of lean protein. They also limit added sugars, refined grains, and many ultra processed snacks, which helps manage blood pressure, cholesterol, and blood sugar (Mayo Clinic).
A simple starting point is to add one more serving of vegetables and swap at least one refined carbohydrate, such as white bread, for a whole grain option each day.
Support weight loss in realistic ways
Weight loss can be an emotional topic, but in the context of metabolic syndrome, even a small shift matters. Both NHLBI and Mayo Clinic stress that losing and keeping off 3 to 5 percent of your body weight can improve insulin resistance and reduce metabolic risk factors (NHLBI, Mayo Clinic).
Instead of focusing on a large final goal, you might:
- Set a short term target of 5 pounds
- Focus on habits you can repeat, like walking after dinner most nights
- Prioritize sleep, since poor sleep can worsen insulin resistance
If you feel stuck, working with a dietitian or health coach can give you structure and accountability.
Address other lifestyle triggers
Cleveland Clinic highlights a few additional lifestyle levers that help manage or even reverse metabolic syndrome (Cleveland Clinic):
- Quit smoking, which damages blood vessels and compounds cardiovascular risk
- Manage stress with methods like breathing exercises, time in nature, or counseling
- Aim for adequate, regular sleep to support hormone balance and appetite control
You do not have to perfect all of these at once. Picking one area and making a small but consistent change can start to move your numbers in the right direction.
When medicines or surgery enter the picture
Lifestyle changes are usually the first step. However, they are not always enough by themselves. In some cases, you and your health care provider might decide to add medication to better control blood pressure, cholesterol, or blood sugar (Mayo Clinic).
For people with obesity related complications who cannot reach a healthier weight through lifestyle changes alone, weight loss surgery might be considered. NHLBI notes that both medicines and surgery can be appropriate when lifestyle steps do not sufficiently manage metabolic syndrome (NHLBI).
Medication is not a failure. It is another tool that, along with your habits, helps lower your long term risk.
You have more influence over your metabolic health than you might realize. Even small, steady changes in movement, food, and sleep can significantly shift your risk.
How to take your next step
If you are wondering whether metabolic syndrome applies to you, the most useful move you can make is to check your numbers. At your next visit, you can ask your provider about your:
- Waist circumference
- Blood pressure
- Fasting blood sugar or A1C
- Triglycerides and HDL cholesterol
If you already know that a few of these are high, you are not alone, and you are not stuck with them. With early attention and a few focused lifestyle changes, metabolic syndrome is often manageable and sometimes reversible (Cleveland Clinic).
You do not need to overhaul your life overnight. You can start with a 10 minute daily walk, a slightly more colorful plate at dinner, or a consistent bedtime. Each small step you take today supports a healthier metabolism, and that is the surprising truth about metabolic syndrome: you have real power to change the story.






